Anal Fissure
Introduction | Symptoms | Treatment | Procedure | Preparation | Recovery
What is an anal fissure?
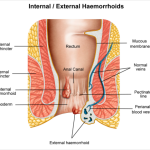
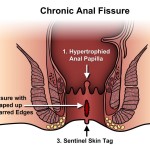
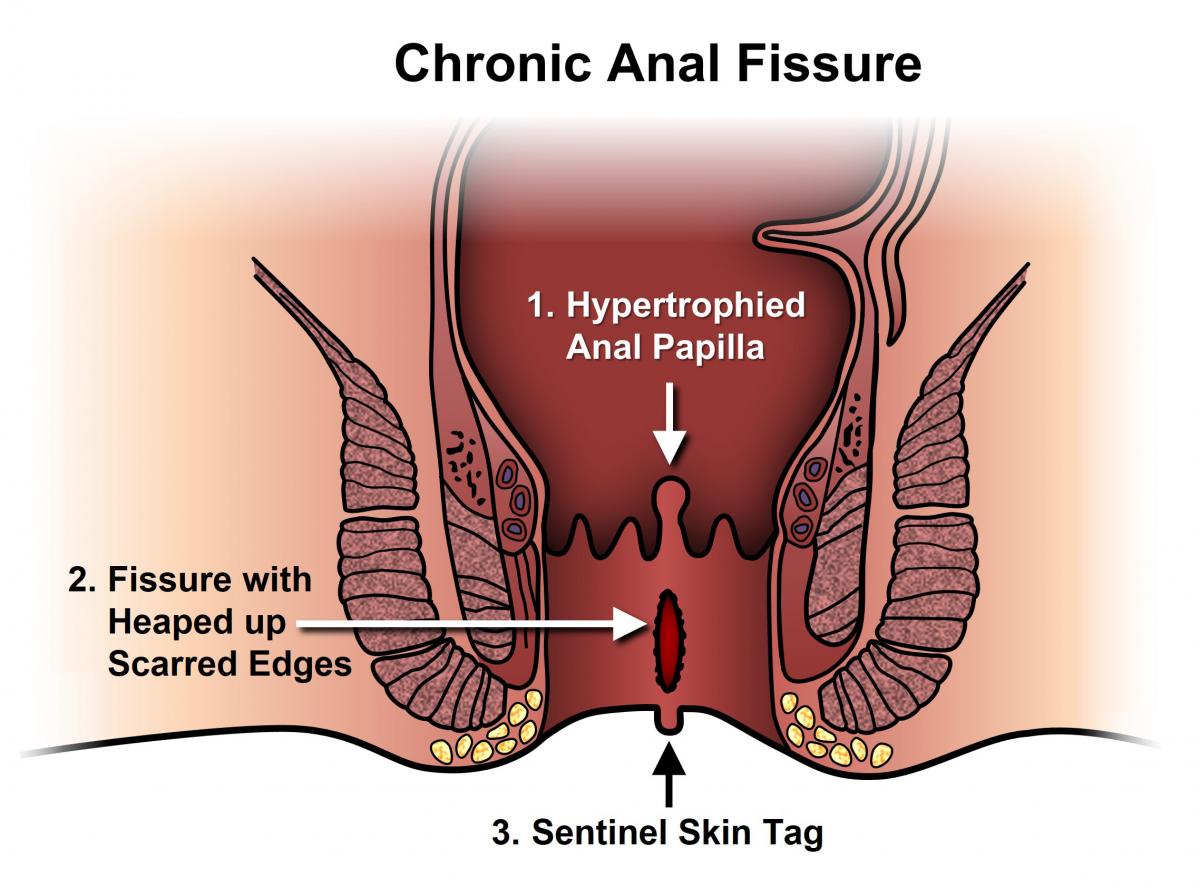
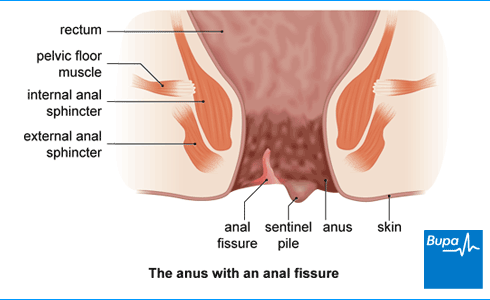
An anal fissure is a split in the skin at the opening of the anus, which leaves exposed some of the muscle fibres of the anal canal. Pain results from the recurrent opening of the wound when the bowels are opened, and it is often accompanied by bleeding. In addition, the inner circle of muscle in the anal canal (called the internal sphincter) goes into spasm: this makes the pain worse and can prevent healing. Anal fissures are different from haemorrhoids and have no relationship with cancer.
What are the symptoms of an anal fissure?
- Pain on passing faeces, which might persist for minutes or hours afterwards. The pain is typically sharp and knife-like rather than an ache.
- Bright-red bleeding when you pass faeces.
- If the fissure is long-standing, a skin tag at the site of the fissure can develop.
What are the treatments for an anal fissure?
- A high-fibre diet: By eating a high fibre diet and drinking plenty of water (6-10 glasses a day), you should aim to keep your motions soft. Sometimes a fibre supplement (such a Fybogel) can help.
- Baths: An ‘ordinary’ 15-minute bath in water as warm as you can tolerate several times daily (or as often as you require) can be very soothing and provide several hours of pain relief.
- Glyceryl trinitrate (GTN) ointment GTN is a relatively new treatment for anal fissures, which acts by relaxing the internal sphincter muscle. This provides pain relief by relieving spasm. It also improves the blood supply to the fissure, which promotes healing in a majority of patients. It is widely accepted by colorectal surgeons to be a valuable alternative to surgery, which has previously been the standard practice. GTN is formulated as a 0.2% ointment, which can be applied three times a day to the skin around the anus and (if possible) a little inside.
The only significant side effect of GTN is that it might cause a headache. If there is no relief of symptoms during a four-week period, then there is little advantage in continuing this form of treatment. - Diltiazem ointment. This is very similar to GTN ointment. It can sometimes be used instead of GTN, or if GTN does not work. Some patients do develop mild skin irritation, which resolves when the cream is discontinued. The cream is also used for a four-week period after which, if the pain persists, surgery may be recommended.
What kind of surgery can be performed for an anal fissure?
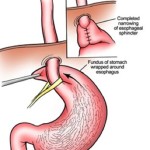
The most commonly used operation to treat anal fissures is called a lateral anal sphincterotomy. It involves a part of the internal sphincter muscle being cut, which relieves the spasm of the muscle, stops the pain and allows the fissure to heal. Occasionally a tag can develop at the inside edge of a long-standing fissure, and this can be removed at the same time. It is not usually necessary to remove or suture the fissure itself. The operation is very effective, but carries a small risk of some change in your ability to control wind from the back passage; in most cases, this problem will resolve completely, but in a small proportion of people, it can be permanent.
Why is surgery necessary for anal fissures?
Surgery is required for some types of fissures that do not respond to simpler forms of treatment.
Is there any special preparation required before the surgery?
In general, anal fissure surgery can be performed on a day-case basis, although occasionally other medical factors or social circumstances might make it necessary for you to stay in hospital. Before your admission, you should be on a high fibre diet and a fluid intake of at least 6-10 glasses of water daily to keep your bowel motion soft.
If you are overweight please try to reduce. This will reduce the anaesthetic risk and optimise your recovery.
What kind of anaesthetic will I have?
Several different kinds of anaesthesia can be used, and the method will be tailored to your particular needs and wishes. With general anaesthesia, you will be asleep for the entire procedure. Some patients are better suited to a spinal or caudal anaesthetic. This is a small injection in the lower back to numb the area so that you will not feel the surgery. With a spinal or caudal anaesthetic, you will be conscious and able to talk to the anaesthetist during the procedure. Some patients who undergo day-case surgery or 23-hour-stay surgery will not require a general anaesthetic.
Pain relief for the surgery:
Sphincterotomy is a very simple operation and many patients experience less pain after their operation than before. However, in order to minimise the discomfort, a number of measures are available:
- At the time of surgery, a local anaesthetic will be injected. This will provide pain relief for much of the day
- After surgery, you will be given painkillers to take by mouth
- You should take baths (a 15-minute bath in water as warm as you can tolerate) several times daily, or as often as you require them. These are very soothing and can provide several hours of pain relief.
How fast will I recover after the operation?
Within one to two hours of your operation, you will be encouraged to get up and walk around. You may eat and drink normally, and (as before) we recommend a high fibre diet and fluid intake of at least 6-10 glasses of water daily. For planned day-case surgery, discharge from hospital will be the same day, or the following day.
You should expect to defecate within one to three days, and this might be uncomfortable at first; a small amount of bleeding is possible. During the first few weeks, you might notice some change in your ability to control wind from the back passage; in most cases, this problem will resolve completely, but in a small proportion of people, it can be permanent. Provided you feel comfortable, there are no restrictions on activity and you may lift things, drive and go back to work.
What should I look out for after the operation?
After your operation, you should contact your Doctor if you notice any of the following problems:
- Increasing pain, redness, swelling or discharge
- Severe bleeding
- Constipation for more than three days, despite using a laxative
- Difficulty in passing urine
- High temperature (over 38ºC) or chills
- Nausea or vomiting