Anal Fistula
What is an Anal Fistula?
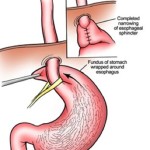
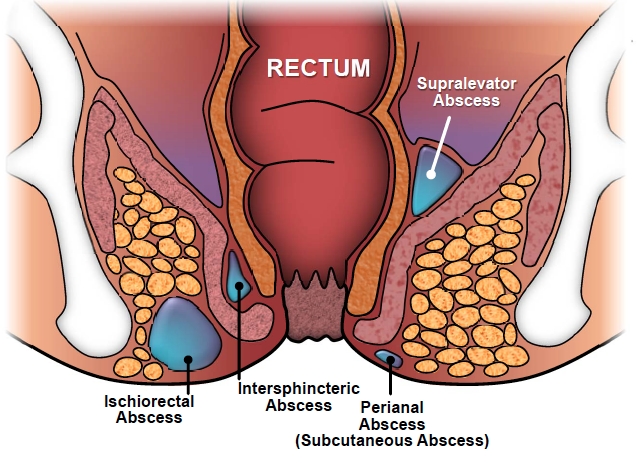
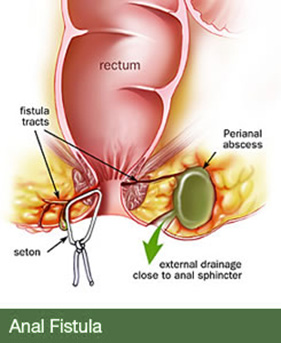
An anal fistula is an abnormal connection between the anus and the skin. On the surface of the skin around the anus, one or more ‘holes’ might be evident. These are the external openings of thin passages that tunnel down towards the anal canal.
What causes an Anal Fistula?
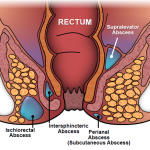
An anal fistula is usually the result of a previous abscess in the area, which has been drained (of pus) but does not fully heal. This results in persistent or intermittent discharge of pus, blood or mucus. Usually, there is no much pain, although an abscess can sometimes recur.
What is the surgery for an Anal Fistula?
Because very few fistulas heal on their own, surgery is needed for almost all patients who have this condition.
What does the operation involve?
Surgery to treat a fistula can be simple or complex (according to the nature of the fistula). Sometimes it is not possible to tell before surgery what is the full extent of the fistula, and so decisions are made while you are anaesthetised. Simple fistulas can be ˜laid open’ by cutting a small amount of the anal skin and muscle to open up the tract. Fistulas that are situated more deeply (complex fistulas) cannot be treated like this because it would involve cutting too much muscle and could result in incontinence. In these circumstances, a variety of other treatments are available – and your surgeon will discuss the options with you individually. Complex fistulas are difficult to treat, and the surgery might be planned in several stages over a period of weeks, months or even years.
What can go wrong after the operation?
Surgery to treat anal fistulas is generally a very safe operation and carries few risks, but (as with any surgical procedure) complications can occur. Since fistulas are closely linked to the muscles that control the passage of faeces and gas, Surgeons are very careful in the decision-making process concerning the nature of the surgery performed because there is a small risk of damage to these muscles. For the majority of patients, the laying open of the fistula does not involve a significant portion of the anal muscles being cut, and the loss of continence is not a risk. Nevertheless, any disturbance of the anal sphincter muscles can lead to some degree of change in the ability to control wind, liquid and, very occasionally, solid faeces from the back passage.
Is there any special preparation prior to surgery?
The details of any operation will be explained to you beforehand. In general, before your admission for surgery, you should be on a high-fibre diet and have a fluid intake of at least 6-10 glasses of water daily. This is to keep your bowel motion soft. You are advised to take 2 tablets of Dulcolax night before your surgery. In some instances, The nurse may give you an enema to empty the bowel (depending on the type of surgery you will have).
If you are overweight please try to reduce. This will reduce the anaesthetic risk and will optimise your recovery.
What kind of Anaesthesia will I have for this operation?
Several different kinds of anaesthesia can be used, and the method will be tailored to your particular needs and wishes. Most patients will require general anaesthesia, and will be asleep for the entire procedure. Some patients are better suited to a spinal or caudal anaesthetic. This is a small injection in the lower back to numb the area so that you will not feel the surgery. With a spinal or caudal anaesthetic, you will be conscious and able to talk to the anaesthetist during the procedure.
What kind of pain relief will be used for the operation?
In order to minimise the pain associated with your operation, a number of measures will be taken:
- At the time of surgery, a local anaesthetic will be injected. This will provide pain relief for much of the day.
- After surgery, you will be given painkillers to take by mouth.
- You should have baths (a 15-minute bath in water as warm as you can tolerate) several times daily, or as often as you require them. These are very soothing and can provide several hours of pain relief.
What should I look out for after the operation?
After your operation, you should contact your Doctor if you notice any of the following problems:
- Increasing pain, redness, swelling or discharge
- Severe bleeding
- Constipation for more than three days, despite using a laxative
- Difficulty in passing urine
- High temperature (over 38ºC) or chills
- Nausea or vomiting
How fast will I recover after the operation?
Within one to two hours of your operation, you will be encouraged to get up and walk around. You may eat and drink normally, and (as before) we recommend a high-fibre diet and a fluid intake of at least 10 glasses of water daily. For a planned day-case surgery, you will be discharged from hospital on the same day, or the following day. You should expect to pass faeces within one to three days, and this might be uncomfortable at first; a small amount of bleeding or discharge is also possible. Over the first few weeks, you might notice some change in your ability to control wind, which should resolve with time. Provided you feel comfortable, there are no restrictions on activity and you may lift things, drive and go back to work.