Colonoscopy and Associated Procedures
What is a colonoscopy?
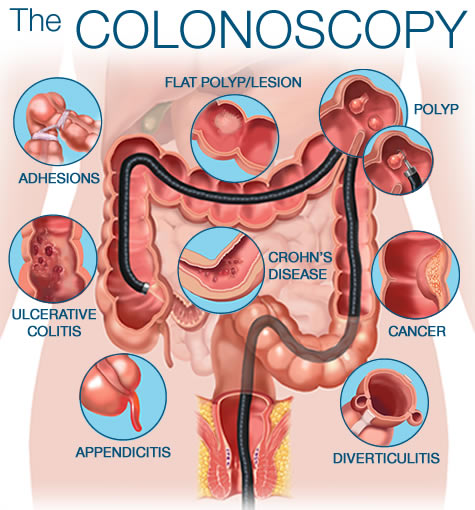
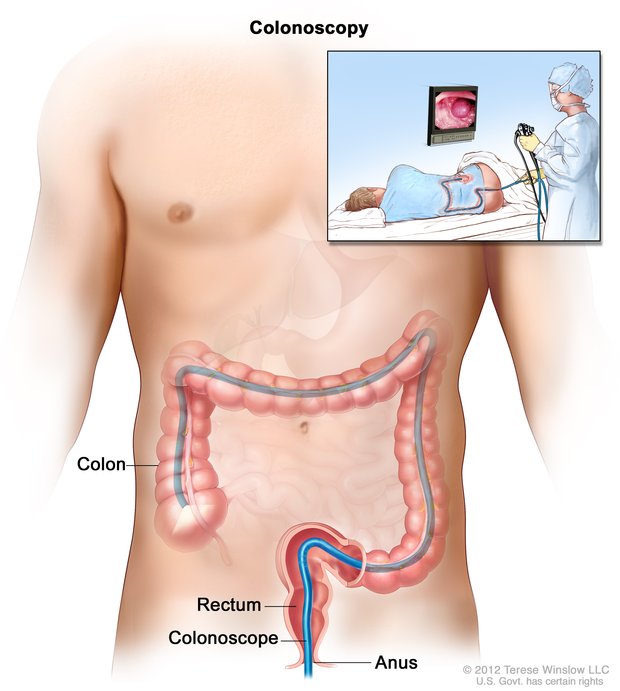
Colonoscopy is a test where your doctor looks into your colon. The colon is sometimes called the large intestine or the large bowel. This procedure allows the doctor to look inside your entire large intestine, from the lowest part, the rectum, all the way up through the colon to the lower end of the small intestine. The procedure is used to diagnose the causes of unexplained changes in bowel habits. It is also used to look for polyps and early signs of cancer in the colon and rectum.
During the procedure, the doctor uses a colonoscopy which is a thin, flexible telescope. It is about as thick as your little finger. The colonoscope is passed through the anus and into the colon. It can the be pushed all the way around the colon as far as the caecum (where the small and large intestine meet).
The colonoscope contains fibre-optic channels which allow light to shine down so the doctor can see inside your colon. It also has a side channel so that the doctor can take small samples (a biopsy) from the inside lining of your colon.
Biopsies do not hurt as the lining of the colon does not have the same pain sensation as your skin. However, you may experience some cramping as air is introduced through the scope and the scope is passed through twisty segments of the colon. The air is needed to allow the doctor to advance the scope along the colon. This may also make you feel bloated and may cause you to pass wind.
Colonoscopy is usually done as an out-patient or day case. Before your procedure you will be asked to change into a hospital gown and lie on your left side with you legs in a curled position. The procedure itself takes around 20-30 minutes. A colonoscopy does not hurt, but it can be a little uncomfortable, particularly when the scope is first passed into the anus.
Why do I need a colonoscopy?
You may be experiencing a change in your normal bowel habit and/or abdominal pain which needs to be investigated. You may be bleeding through your back passage or you may have anaemia (low blood count), for which your doctor needs to find the cause.
We may diagnose diverticular disease (small pockets that are created in the lining of the colon). This can be controlled with diet and mediction.
The diagnosis may be haemorrhoids (piles), which can sometimes be treated during colonoscopy, depending on severity.
A colonoscopy is sometimes carried out to see if you have a polyp (innocent growth) that can be removed during colonoscopy. If polyps are found you may need to have a repeat colonoscopy at a later date to check for recurrence.
Sometimes a colonoscopy is carried out to see if you have a tumour, following which you may need to have an operation.
To confirm or exclude crohns disease, colitis and tumours, biopsies will normally be taken and sent to the laboratory for testing.
Photographs may be taken of the inside of your colon.
Tumours of the colon can run in families, therefore, if this is known to be the case, you may be advised to have a colonoscopy on a regular basis. We do this because colon tumours are curable if caught early.
Whatever the findings, the colonoscopy will allow for an accurate diagnosis to be made and helps to provide treatment that will be suitable to you.
Preparation for the procedure
To allow a clear view, whole colon must be completely empty of waste material. It is essential that you drink the 3 sachets of fleet that the doctor prescribes for you and to drink plenty of clear fluids. You will be provided with an information sheet on how to take the medicine.
What are the risks and complications?
Most colonoscopies are done without any problems. If you have had a sedatve you may feel tired or sleepy for several hours afterwards. You may pass a small amount of blood from your anus if a biopsy was taken, or a polyp removed, Occasionally the colonoscope may cause damage to the colon. This may cause bleeding, infection and rarely, perforation. If any of the following occur within 48 hours after a colonoscopy, it is important that you consult your doctor immediately:
- Abdominal pain. In particular if it becomes gradually worse, and is different or more intense than any usual pains you may have had previously
- Fever
- Passing a lot of blood from your anus
