Diagnostic Laparoscopy
What is Diagnostic Laparoscopy?
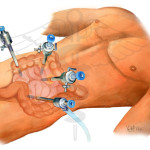
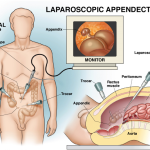
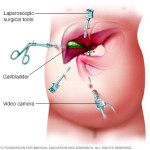
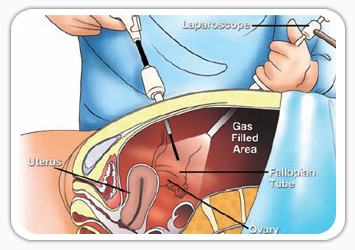
A laparoscope is a telescope designed for medical use. It is connected to a high intensity light and a high-resolution television camera so that the surgeon can see what is happening inside of you. The laparoscope is put into the abdominal cavity through a hollow tube and the image of the inside of your abdomen is seen on the television screen. In most cases, this procedure (operation) will be able to diagnose or help discover what the abdominal problem is.
Why is Diagnostic Laparoscopy performed?
- Abdominal pain:
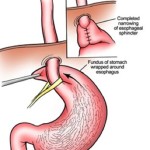
Laparoscopy has a role in the diagnosis of both acute and chronic abdominal pain. There are many causes of abdominal pain. Some of these causes include appendicitis, adhesions or intra-abdominal scar tissue, pelvic infections, endometriosis, abdominal bleeding and, less frequently: cancer. It is used in patients with irritable bowel disease to exclude other causes of abdominal pain. Surgeons can often diagnose the cause of the abdominal pain and, during the same procedure, correct the problem. - Abdominal mass:
A patient may have a lump (mass or tumour), which can be felt by the doctor, the patient, or seen on an X-ray. Most masses require a definitive diagnosis before appropriate therapy or treatment can be recommended. Laparoscopy is one of the techniques available to your physician to look directly at the mass and obtain tissue to discover the diagnosis. - Ascites:
The presence of fluid in the abdominal cavity is called ascites. Sometimes the cause of this fluid accumulation cannot be found without looking into the abdominal cavity, which can often be accomplished with laparoscopy. - Liver disease:
Non-invasive X-ray imaging techniques (sonogram, CT scan and MRI) may discover a mass inside or on the surface of the liver. If the non-invasive X-ray cannot give your physician enough information, a liver biopsy may be needed to establish the diagnosis. Diagnostic laparoscopy is one of the safest and most accurate ways to obtain tissue for diagnosis. In other words, it is an accurate way to collect a biopsy to sample the liver or mass without actually opening the abdomen. - “Second look” procedure or cancer staging:
Your doctor may need information regarding the status of a previously treated disease, such as cancer. This may occur after treatment with some forms of chemotherapy or before more chemotherapy is started. Also, information may be provided by diagnostic laparoscopy before planning a formal exploration of the abdomen, chemotherapy or radiation therapy.
What tests are necessary before Laparoscopy?
Ultrasound may be ordered by your doctor as a non-invasive diagnostic test. In many cases, information is provided which will allow your surgeon to have a better understanding of the problem inside your abdomen. This test is not painful, is very safe, and can improve the effectiveness of the diagnostic laparoscopy.
A CT Scan (X-ray)may be ordered which uses computers to visualize the intra-abdominal contents. In certain circumstances, it is accurate in making the diagnosis of abdominal disease. It will allow your surgeon to have a “road map” of the inside of your abdomen. A radiologist may use a CT scan to place a needle inside your abdomen. This is known as a CT guided needle biopsy. This will often be done before a diagnostic laparoscopy to decide if laparoscopy is appropriate for your condition.
An MRI (magnetic resonance imaging) may be ordered to view the inside of the abdominal cavity. It is not required for most abdominal problems, but may be necessary for some. Routine blood test analysis, urinalysis, and possible chest X-ray or electrocardiogram may be needed before diagnostic laparoscopy. Your physician will decide which tests are necessary and will review the results of those tests, which have already been performed.
What type of Anaesthesia is used?
Diagnostic laparoscopy is performed either under local anesthesia with sedation or with general anaesthesia. With your help, your surgeon and an anaesthesiologist will decide on a method of anesthesia to perform safe and successful surgery.
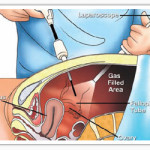
LOCAL: Anaesthesia can be injected into the skin of the abdominal wall to completely numb the area and allow safe placement of a laparoscope. Most patients feel a short-lived “bee sting” that lasts a second or two. Small doses of intravenous sedation are given at the same time allowing the patient to experience what is known as “twilight” sleep in which patients are arousable but asleep. Once an adequate depth of sleep is reached and local anaesthesia administered, gas is placed into the abdominal cavity. This is called a pneumoperitoneum. The patient may experience a bloated feeling. The gas is removed at the end of the operation. The two most common gases used are nitrous oxide (“laughing gas”) or carbon dioxide. There is very little risk of ill-effects of the gas.
GENERAL: Anaesthesia is given to those patients who are not candidates for “twilight” sleep or who want to be completely asleep. General anaesthesia may be preferable in patients who are young, who cannot lie still on the operating table, or have a medical condition that is safer to perform in this manner. Some patients end up having a general anaesthesia even though they prefer local anesthesia with sedation, as the appropriate anaesthesia for laparoscopy differs from patient to patient.
What preparation is required?
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- It is acceptable to shower the night before or morning of the operation .
- Most diagnostic laparoscopy procedures are performed as an outpatient; meaning you will go home the same day the procedure was performed .
- You should have nothing to eat or drink for six to eight hours before the procedure.
- Standard blood, urine, or X-ray testing may be required before your operative procedure. This will depend on your age and medical conditions.
- Report to the hospital at the correct time, which is usually 1-2 hours earlier than your scheduled surgery.
- If you take medication on a daily basis, discuss this with your surgeon prior to surgery as you may need to take some or all of the medication on the day of surgery with a sip of water.
- If you take aspirin, Vitamin E, blood thinners or arthritis medication, discuss this with your surgeon so they can be stopped at the proper time before your surgery.
- You will need to ask your surgeon what specifically is required in preparation for your surgery.