Laparoscopic Cholecystectomy
What is a laparoscopic cholecystectomy?
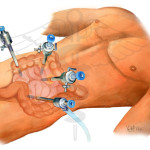
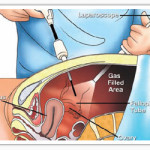
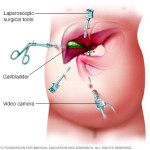
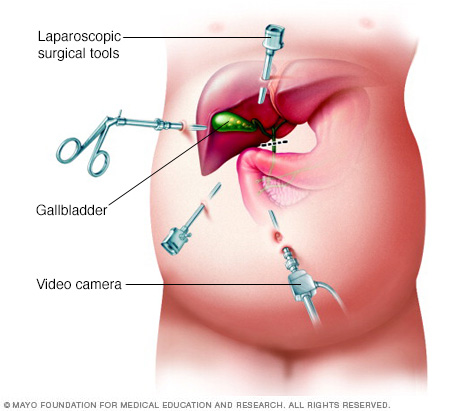
Laparoscopic cholecystectomy is a surgical procedure in which the doctor removes your gallbladder with the aid of a laparoscope. The gallbladder is a small pear-shaped organ on the underside of the liver that is used to store bile.A laparoscope is a small telescope, which is attached to a small camera and light source to enable the internal abdominal cavity to be visualized on a television screen. Three or four small (less than a cm each) incisions are made into the abdomen, through which the telescope and laparoscopic instruments are inserted. Gas is passed into the abdominal cavity to inflate it, so that the gallbladder can be seen more easily. Laparoscopic (Keyhole) cholecystectomy is the most common way to remove the gallbladder today, but you should always keep in mind that cholecystectomy may not always be possible laparoscopically anda larger incision maybe needed to remove the gallbladder (open cholecystectomy technique).On the other hand, it is now also possible to perform cholecystectomy with a single small incision at the umbilicus (belly button). This new technique is known as SILS (single incision laparoscopic surgery). SILS cholecystectomy gives superior cosmetic results compared to even traditional laparoscopic cholecystectomy. You can ask us if you are a candidate for SILS cholecystectomy.
What does the gallbladder do?
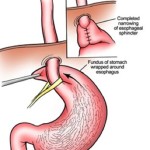
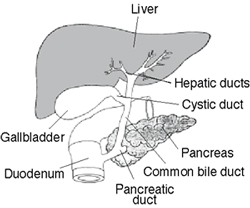
The liver produces a substance called bile. This is a green coloured liquid that helps the body to digest fats. Bile contains water, cholesterol, fats, bile salts and bilirubin. Bile salts break up the fat, and bilirubin gives stools their yellow-brown colour. The liver secretes bile into a branching network of small tubes called bile ducts, which join together to form a single large tube called common bile duct. The common bile duct opens into the duodenum, which is the initial part of the intestine just beyond the stomach. The gallbladder is connected to the common bile duct. Thus the bile flows from the liver to the common bile duct and into the gallbladder where it is temporarily stored when we are fasting. After we take a meal, the gallbladder contracts and empties bile into the duodenum where it helps to break down the fats.
What are gallstones?
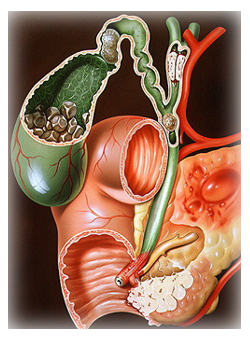
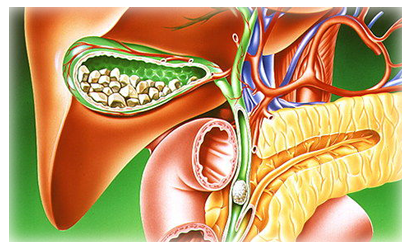
Gallstones are formed when the bile stored in the gallbladder hardens into pieces of stone-like material. Gallstones are mainly composed of cholesterol. Most patients with gallstones remain symptom-free for many years and may, in fact, never develop any symptoms. Symptoms of gallstones are variable ranging from brief episodes of abdominal pain (known as biliary colic) to potentially life-threatening complications, such as acute inflammation and infection of the gallbladder (cholecystitis), inflammation of the pancreas (pancreatitis) and obstructive jaundice. It is accepted that the best treatment for gallstones that cause symptoms is the removal of the gallbladder by keyhole surgery (laparoscopic cholecystectomy). Occasionally surgery may be recommended for patients with gallstones in the absence of symptoms also.
When is a laparoscopic cholecystectomy done?
This procedure is performed when you have stones or inflammation in your gallbladder, causing pain. The gallbladder is shaped like a pear. It is attached to the undersurface of the liver. Bile produced in the liver is stored in the gallbladder. Concentrated and stagnant bile can form sediment in the gallbladder that can turn into gallstones. These stones may remain loose in your gallbladder or they may block the gallbladder outlet causing pain when the gallbladder contracts. In that case, the gallbladder may also become swollen, inflamed, and/or start (rarely) to decompose (become “gangrenous”). There are no alternatives to surgically removing the gallbladder when it is causing pain.
Complications of Gallstones
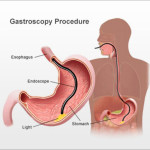
Gallstones that are confined to the gallbladder usually only cause intermittent episodes of pain, known as biliary colic. When a stone blocks the exit of the gallbladder the flow of bile is occluded, which can cause infection and inflammation of the gallbladder, called acute cholecystitis. A patient with acute cholecystitis may have a fever, severe upper right-sided abdominal pain and may vomit. When gallstones enter the common bile duct they can cause jaundice, cholangitis and pancreatitis. The stone blocking the flow of bile into the intestine causes jaundice. This leads to absorption of bilirubin into the bloodstream – causing yellow pigmentation of the skin and eyes. This absorbed bilirubin is excreted in the urine and gives it a dark yellow color. The obstruction of the common bile duct by a stone can also lead to infection in the biliary system. This is known as cholangitis. This infection can reach the liver if not treated promptly, and can result in inflammation of the liver and eventually liver abscesses. Pancreatitis occurs when a gallstone passing through the bile duct occludes the pancreatic duct leading to inflammation of the pancreas. The pancreatitis usually resolves if the gallstone passes out spontaneously into the duodenum. However, about 10 percent of patients with pancreatitis develop severe complications. Presence of gallstones in the common bile duct can be confirmed by doing an MRI of the abdomen known as MRCP (magnetic resonance cholangio-pancreatography) Common bile duct stones have to be removed in addition to removal of the gallbladder. These can be removed by an endoscopy performed by inserting a flexible tube through your month into your duodenum where the common bile duct opens followed by removal of gallstones in the common bile duct. This is known as endoscopic retrograde cholangio-pancreatography (ERCP). ERCP is usually done prior to laparoscopic cholecystectomy. Occasionally it can be needed after the surgery if there is a stone detected in the common bile duct later. It is also possible to remove stones in the common bile duct surgicallyduring the laparoscopy procedure. This is known as laparoscopic common bile duct exploration. It is usually done for large stones in the common bile duct or when ERCP fails to remove stones Rare complications of gallstones include perforation of the gallbladder, erosion of the gallbladder into the bowel (cholecysto-enteral fistula) and passage of a gallstone into the bowel leading to a bowel obstruction. Occasionally due to certain difficulties encountered during laparoscopic cholecystectomy, the surgeon may prefer to convert to open cholecystectomy. The inflamed gallbladder is sometimes stuck to surrounding organs or there may be excessive bleeding during the surgery and therefore the surgeon may choose to perform an open cholecystectomy if he/she feels it is safer for the patient. Since this procedure is more invasive and leaves a larger scar, you will have a longer stay in hospital.
Benefits of this type of Surgery
Having a laparoscopic cholecystectomy means that you will have a shorter recovery time, less pain, shorter hospital stay and will be able to return to work more quickly. With the laparoscopic cholecystectomy, you will probably have to stay in the hospital only for a day or two. On the other hand, an open cholecystectomy may increase your hospital stay to approximately 5 days. Also, because the incisions are much smaller with the laparoscopic technique you will find that the pain you experience will be a lot less than if you had the traditional open cholecystectomy.
What to expect before the surgery
Usually the doctor will get a set of routine blood investigations and other specific blood tests known the as the liver function test. They will be accompanied by an Ultrasound of the abdomen if it has not been previously done. Based on the evaluation and interpretation of the above results the doctor will decide whether you have any other complications related to the gall stones as stated above. Once the surgery is confirmed, You are required to be fasting for 6-8 hrs prior to the surgery. Any medication for the blood pressure or diabetes has to be taken as per the instructions of the doctor on the day of the surgery. You will be admitted in the hospital and prepared for the surgery (removal of hair in the area where the surgery is to be performed). Later you will get an injection (prophylactic antibiotic) about half an hour before being wheeled in the operation theatre.
Risks and Complications
Serious complications arising from laparoscopic cholecystectomy are uncommon. All types of surgery are associated with a certain degree of risk and it is important that these risks are explained fully to the patient in order for an informed decision to be made. The risks are related both to anesthesia andthe surgery itself.
- There is small risk of injury to the bile duct
- Injury to internal organs
- Injury to major blood vessels
- There is a small risk of bleeding, infection and hernia formation
- In the event of a stone(s) being found in the bile duct there is a slight chance that further procedures (such as ERCP) will be requireded
- There is a 1% to 3% risk that keyhole surgery may need to be converted to an open gallbladder operation. The chances of this are higher in complex cases and patients who have had previous abdominal surgery.
After the Surgery
You will normally be able to resume normal daily activities after one week. It is important that you follow your doctor’s instructions. You may experience mild to moderate pain and it is important that you take your pain medication as prescribed. Nausea and vomiting are not uncommon after this type of surgery and your doctor can prescribe medication to help relieve these symptoms. If these symptoms persist then you should inform your doctor. About 20% of people will have transient diarrhea after having their gallbladder removed. Eating plenty of high fiber foods can help absorb excess water and make bowel movements more bulky. Occasionally a short course of medications may be required.
When to Call the Doctor
It is important that you inform your doctor if you experience any of the following symptoms after your surgery:
- Fever
- Pain that is not relieved by medication
- Redness and pain at the wound site
- Any pus or discharge from wound
- Bleeding
- Persistent cough or shortness of breath
- You are unable to tolerate fluids and diet
- Persistent nausea and/or vomiting
- Chills
- Increased abdominal swelling.