Overview on Obesity
Overweight and Obesity are defined as abnormal or excessive fat accumulation that may impair health.
The fundamental cause of obesity and overweight is an energy imbalance between calories consumed and calories expended.
Modern lifestyle promotes Obesity in many ways.
- An increased intake of energy-dense foods that are carbohydrate-rich and contain saturated fats
- A decrease in physical activity due to the increasingly sedentary nature of work in many occupations
- Ease of transportation
- Lack of opportunity to exercise
Minority of cases is due to medical causes such as endocrine system malfunctions and a few have genetic cause for Obesity.
Body mass index (BMI), defined as a person’s weight in kilograms divided by the square of his height in meters (kg/m2), is generally used as the parameter to grade the severity of Obesity. However, it should be considered a rough guide because it may not correspond to the same degree of fatness in different individuals.
According to the World Health Organization (WHO) definition,
Overweight: BMI greater than or equal to 25
Obesity: BMI greater than or equal to 30
Clinically Severe Obesity: BMI greater than or equal to 40
Super Obesity: BMI greater than or equal to 50
Calculate your BMI here – (BMI Calculator)
Health consequences of Overweight and Obesity:
Obesity is a major risk factor for noncommunicable diseases such as,
- Cardiovascular diseases (mainly heart disease and stroke), which are the leading causes of death even in younger people
- Type 2 Diabetes Mellitus
- Musculoskeletal disorders (especially Osteoarthritis)
- Some Cancers (including endometrial, breast, ovarian, prostate, liver, gallbladder, kidney, and colon)
- Asthma
- Gastro Esophageal Reflux Disease (GERD)
- Fatty Liver
- Infertility
- Psychosocial Morbidities
On average, obesity reduces life expectancy by six to seven years, a BMI of 30–35 kg/m2 reduces life expectancy by two to four years,[36] while severe obesity (BMI > 40 kg/m2) reduces life expectancy by ten years.
Managing Obesity
Obesity is mostly preventable through a combination of social changes and personal choices. For someone who is already obese, changes to diet and exercising are the common pathways. These can be achieved in several manners, depending upon the suitability, determined by an evaluation of the weight, personal circumstance and the overall medical status of the individual.
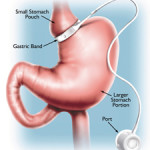
Diet quality can be improved by reducing the consumption of energy-dense foods, such as those high in fat and sugars, and by increasing the intake of dietary fiber. Medications may be taken, along with a suitable diet, to reduce appetite or decrease fat absorption. If diet, exercise, and medication are not effective, a gastric balloon or surgery may be performed to reduce stomach volume or bowel length, leading to feeling full earlier or a reduced ability to absorb nutrients from food.
Currently, the available options are
A supervised diet and exercise program
Physician supervised medical therapy
Endoscopic treatments
Non Endoscopic treatments
Surgical weight loss
Obesity and Diabetes
There is a direct relationship between Obesity and Diabetes Mellitus Type II. It is known that around 20% of severely obese patients develop Diabetes.
Diabetes is marked by high levels of sugar (glucose) in the blood and occurs when the body does not respond correctly to insulin, a hormone released by the pancreas. An obese person has double the risk of developing diabetes, and a severely obese person is at a tenfold increased risk. The risk of developing diabetes also increases with age, family history and obesity localized more in the abdomen (central obesity). Consumption of fatty and high-carbohydrate foods leads not only to obesity, but also to a higher amount of fatty acids in the blood and a buildup of lipids in the liver and skeletal muscles, causing resistance to insulin and consequently diabetes.
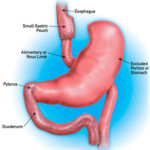
Control of Diabetes through Bariatric Surgery
The Surgical procedures that have been used so far, purely with an intention to reverse Obesity, have found a new indication- the resolution of Diabetes. Therefore, it’s only reasonable that they could be recommended purely for this indication, especially for those with poorly controlled diabetes, even if weight loss is not the objective.
Bariatric surgery has been shown to improve or resolve type 2 Diabetes. Immediately after surgery, blood sugar levels improve and diabetic medications can be stopped. This happens even before significant weight loss. Recent studies show that this is due to changes in the gut hormones which control metabolism and a consequent change in fat and muscle cell metabolism which lead to improvement of insulin resistance.
About 80 percent of obese patients who undergo Roux- EN-Y Gastric Bypass/Sleeve Gastrectomy are free from diabetes one year after surgery. These results are typically persistent for the rest of life, as long as a healthy body weight is maintained. Patients who have a milder form of diabetes (controlled with diet) for less than five years, and who achieve greater weight-loss after surgery, are more likely to also achieve complete resolution of diabetes. Weight loss following gastric bypass in obese non-diabetic patients decreases their likelihood of developing diabetes by 60 percent over four years.
THE EARLIER THE SURGERY, THE BETTER THE RESULTS
The Earlier the Surgery, the Better the Results
The longer a patient has diabetes, the greater the likelihood of irreversible loss of insulin production. A key finding of all studies is that the less time one suffers from diabetes; the more likely he or she will have complete remission of diabetes following surgery.