Thyroid Surgery
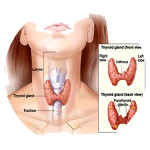
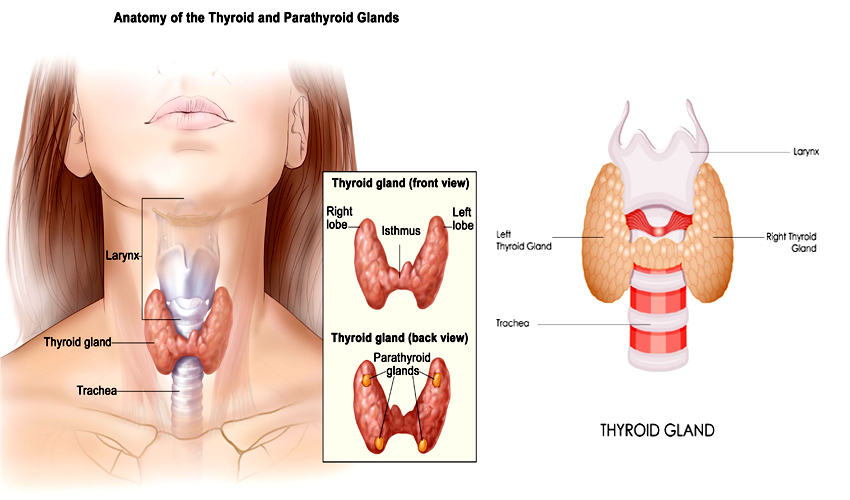
Thyroidectomy is the removal of all or part of your thyroid gland. Your thyroid is a butterfly-shaped gland located at the base of your neck. It produces hormones that regulate every aspect of your metabolism, from your heart rate to how quickly you burn calories.
Usually a patient is clinically evaluated by a Physician and/or an Endocrinologist. Patients often present with either an enlargement of the thyroid gland known as a ‘Goitre’ or the presence of a nodule which is seen on ultrasound imaging of the thyroid gland.
If blood tests have shown that the function of the thyroid gland is normal, then the clinician or the surgeon proceeds to investigate the nature of the nodule. For this, a fine needle aspiration cytology (FNAC) is taken from the nodule. In this procedure, a small needle is inserted into the nodule (under ultrasound guidance), and a small amount of fluid is aspirated (drawn up into a syringe), which is sent to the laboratory for diagnosis. This will determine the nature of the thyroid nodule and decide any further course of action.
Indications for Thyroidectomy
A thyroidectomy may be recommended for conditions such as:
- Thyroid cancer
Cancer is the most common reason for thyroidectomy. If you have thyroid cancer, removing most, if not all of your thyroid will likely be a treatment option.
- Non-cancerous enlargement of the thyroid (goitre)
Removing all or part of your thyroid gland is an option if you have a large goitre that is uncomfortable or causes difficulty breathing or swallowing, or in some cases, if the goitre is causing hyperthyroidism (overactive thyroid gland.)
- Overactive thyroid (hyperthyroidism)
Hyperthyroidism is a condition in which your thyroid gland produces too much of the hormone thyroxine. If you have problems with anti-thyroid drugs and do not wish to receive radioactive iodine therapy, thyroidectomy may be an option.
Risks and complications after the surgery
Potential complications include:
- Bleeding
- Airway obstruction caused by bleeding
- Permanent hoarse or weak voice due to nerve damage
Damage to the four small glands located behind your thyroid (parathyroid glands), which can lead to hypoparathyroidism, resulting in abnormally low calcium levels in your blood and bones and an increased amount of phosphorus in your blood.
Surgical Procedure
During thyroidectomy
Surgeons perform thyroidectomy using general anaesthesia, so you are unconscious during the procedure. The anaesthesiologist or anaethetist administers an anaesthetic medication either as a gas by breathing it through a mask, or as a liquid which is inserted into a vein located in your hand or arm.
The surgical team places several monitors on your body to help make sure that your heart rate, blood pressure and blood oxygen remain at safe levels throughout the procedure. These monitors include a blood pressure cuff on your arm and heart-monitor leads attached to your chest.
Once you are unconscious, the surgeon makes a small incision in the front of your neck, and all or part of the thyroid gland is removed, depending on the reason for the surgery. If you are having a thyroidectomy as a result of thyroid cancer, the surgeon may also examine and remove lymph nodes around your thyroid. Lymph nodes are known to be involved in the spread of cancer to other parts of the body, so it is for this reason that they are removed. Thyroidectomy usually takes several hours.
Following surgery, you are moved to a recovery room where the health care team monitors you for complications from the surgery and anaesthesia. Once fully conscious and comfortable, you will be transferred to the ward where you will be continued to be closely monitored. You may have a drain insitu under the incision in your neck. This drain is usually removed the morning after surgery.
You will be able to eat and drink as usual after surgery. Your throat may be sore and your voice hoarse. Most people who have thyroidectomies remain in the hospital for about 24 hours. When you go home, you can usually return to your regular activities, often within a few weeks. Talk to your doctor about specific activity restrictions.